Hallux Valgus

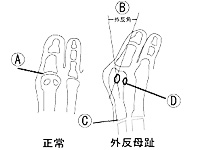

Hallux valgus is defined as the hallux adducted at the metatarsophalangeal joint (MTP joint) (Fig.1a)with a hallux valgus angle(Fig.1b) of approximately 15 to 18 degrees.
Since it may involve severe pain and cause impairment of walking, it is thought that it becomes the source of indefinite complaints of the whole body (stiff neck, low back pain, knee joint pain, and headache).
- ◎Causes
-
The development of hallux valgus is related to several causes:
(1) Hereditary anatomical factors:
The Egyptian forepart of the foot, where the hallux is longer than the second toe
Strong metatarsal varus at the tarsometatarsal joint of the first metatarsal bone(Fig.1c)
The sesamoid bone(Fig.1d) to the side of a tibia is defected or is smaller than the sesamoid bone to the side of a fibula.(2) Environmental factors that affect feet from outside
The forepart of the foot is tightly squeezed in closed footware (ill-fitting tabi, stockings, socks, high heels, and pumps).
Sports that may impose burdens on the forepart of the foot (tennis, skiing, table tennis, track and field, etc.)(3) Other factors
Vulnerability of connective tissue and sex hormones
Complication of diseases (rheumatism etc.) - ◎Prevention and Measures
-
First of all, minimize the factors from outside.
Avoid pointed shoes, and choose shoes that fit your feet. (This may be difficult, and we will offer consultation.)
On regular basis, try to exercise and massage feet while and after taking a bath.●Open and close the toes.
●Shake the hand with the toes.
●Drag a tower in a sitting posture.
●Grab a small ball of about 3 centimeters in diameter with the toes.
●Hang a rubber band over both halluces and open your legs from side to side.It is important to develop the muscles of the toes and the whole feet by yourself, so that valgus may not be worse than now.
Hammertoes

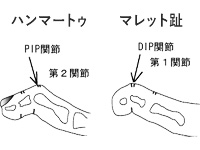
Two major symptoms are hammertoes, where the toes are bent at the PIP joint and extended at the DIP joint, and mallet toes, where the toes are bent and deformed at the DIP joint.
You may often experience pain when taking off shoes, and calluses are often formed at the backside of the deformed toe PIP joint and at the bottom area of metatarsal heads (below the base of the toes).
- ◎Causes
-
(1) Some toes are congenitally long.
(2) The regular use of ill-fitting shoes and stockings (shoes with no room in the forepart of the foot, shoes in which the foot easily slips to the front, oversized shoes, marvelously elastic stockings).
(3) Diseases that easily accompany the deformed toes (rheumatic arthritis, diabetes, gout, other neurological disorders, muscular paralysis, etc.).
- ◎Prevention and Measures
-
Avoid ill-fitting shoes and stockings, and choose shoes that fit your feet.
Minor hammertoes may be corrected by pulling toes. Gently extend and rotate the bent joint while taking a bath with patience.
Spread Foot

While the forepart of the foot spreads out in a fan-like form and the transverse arch is lost, the load of the bottom area of metatarsal heads (below the base of the toes) in the second and third toes(Fig.2) easily causes the severest pain while walking.
- Causes
-
(1) Due to working, vigorous sports, and the regular use of high heels, body weight is put on the forepart of the foot, and the load of the metatarsophalangeal joint (MTP joint)(Fig.1a) increases.
(2) It develops on the foot with hallux valgus or pes plano-valgus.
(3) Due to chronic rheumatoid arthritis (damage and relaxation of the joint and the ligament) etc.
- Prevention and Measures
- Low-heeled shoes that may not impose burdens on the MTP joint and that have soft insole materials are good, and those with shoelaces or buckles to avoid slips inside are preferable. The use of sole plates, massage, and toe exercise are also important.
Hallux Rigidus
The range of motion of hallux at the MTP joint is restricted, you may experience pain particularly when it is dorsiflexed, and calluses amd corns are easily formed at the bottom of the hallux.
As stepping motion becomes difficult while walking, it can be said that body weight is shifted outside of the foot, and that the unnatural walking may cause other disorders.
- Causes
-
(1) Congenital factors.
(2) The use of tight shoes.
(3) After traumas; arthritis such as chronic rheumatoid arthritis, gout, and psoriasis
- Prevention and Measures
- Avoid wearing tight shoes.
In addition, the use of shoes that enable us to exercise every part of the body only by shifting body weight and the use of metatarsal pads can reduce burdens on the hallux.
In case of minor hallux rigidus, the administration of anti-inflammatory drugs and steroid works for pain, but fixing in plaster or an operation may be necessary. Please consult your orthopedist.
Flat Foot
Due to the pathological decrease of the sole medial longitudinal arch, you experience pain, physical capabilities are reduced, and you get exhausted easily.
A lot of burdens are imposed on the second and third bottom area of metatarsal heads (below the base of the toes), and calluses may be formed in the plantar part.
- Causes
- (1) Acquired flat foot in childhood: It is often found among children, and is due to lack of exercise and delayed development.
(2) Idiopathic pes plano-valgus: Weight gain due to obesity or pregnancy, and weakening of ligament or muscle.
(3) Degenerative diseases and hereditary diseases. - Prevention and Measures
- For flat foot in infancy, exercises including standing on tiptoe, such as playing barefooted, tree climbing, and jump roping, are necessary.
For flat foot in adulthood, exercises that strengthen muscles and tendons forming such arches as tibialis posterior muscle and plantar muscles, like dorsiflexion exercises of the hallux, are effective.
Insertion of arch support is also effective, but you should know that insertion might cause other disorders.
*False flat foot: It refers to a condition where there appears to be no plantar arch due to the unusual development of muscles or excessive fat while lowering of arch is not found. You can do sports or walk with no problem.
High Arch
In the foot with a high instep in which the arch is higher than usual, calluses are easily formed in the bottom area of metatarsal heads.
- Causes
- Causes cannot be identified, but shoes could not be the cause.
- Prevention and Measures
- As burdens are easily imposed on the bottom area of metatarsal heads (Fig.2), shoes with as low heels as possible are recommended.
* There is no standard for the height of arch, and it is hereditary. Too high an arch or too low an arch cannot always be abnormal, and it is often that height causes no functional disorder.
Achilles peritendinitis
Swelling, pain, and, sometimes, squeak noise are observed around the Achilles tendon, and they may cause disorders in walking.
Characteristically, pain often emerges when walking downhill or going down the stairs, and it is strong at the onset of motion.
- Causes
- (1) It develops after repetitive motions to the Achilles tendon in sports and working cause excessive burdens.
(2) The use of ill-fitting shoes. - Prevention and Measures
- You are required to lie quietly in bed for the acute symptoms, and to control motion of the Achilles tendon.
You may need to reduce burdens on the tendon while walking by raising the heel area with the help of shoes and plantar plates. Warm-up exercises and stretching before and after doing sports are important for prevention. Also, shoes should be reexamined.
Plantar Fasciitis
It is a disorder of the fascia, called plantar aponeurosis(Fig.5), that covers muscles longitudinally expanding in the middle of the sole, and inflammation develops in the heel area when repetitive motions such as running, jumping, and walking impose excessive burdens on the plantar aponeurosis.
Major symptoms include pain in the heel area on motion and while walking, and, when it becomes severe, it will be difficult to contact ground at the heel area.
- Causes
- As for sports-related causes, it often develops among joggers and long-distance runners, and it also develops among the middle-aged or elderly while walking for a long time or working without sitting since such activities impose a lot of burdens on plantar aponeurosis.
- Prevention and Measures
- Keeping the area at rest is the most important.
Use icing and compresses for anti-inflammation, and restrict walking, running, and jogging.
Also be careful for obesity that is one of the excessive burdens on the plantar aponeurosis.
Calluses and Corns

They are slightly raised, round or elliptical thickened keratin with a blurred boundary; the sense of touch is poor, and the skin yellowish. They sometimes accompany pain.
Unlike calluses, they have a clear boundary with the normal skin and have a nucleus in the middle.
Characteristically, the surface of the skin is raised to form calluses, whereas corns cut into the skin, and they accompany stronger pain than calluses while walking.
They often develop in the areas where pressure concentrates, such as the pointed toe area, the inter-toe area, and the bottom area of metatarsal heads.
When you untreat them for a long time or treat them by yourselves inappropriately, they may inflame inside and suppurate.
- Causes
- (1) Pressure on the skin and stimuli including frictions, due to the change of arch structure and the increase of body weight.
(2) Stimuli by the shoes that receive excessive pressure or those with a hard sole.
(3) Characteristic stimuli by sports, working, etc. - Prevention and Measures
- The best way is to remove both calluses and corns.
At the same time, avoid shoes that give excessive pressure or shoes with hard soles.
They often develop from the imbalance of bones, and exercise in the toes is important to build muscle.
Warts (Viral Verruca)

Warts are called verruca in the medical term. Most of them are infectious diseases that papillomavirus causes, and they primarily develop in hands and the sole.
The surface of the raised skin with black dots has capillary vessels inside, and it will bleed when it is cut.
Warts accompany pain when they develop in the sole.
- Causes
- Infections from others or those from exudates that you made.
- Prevention and Measures
- Immediately see a dermatologist for treatment.
Be careful that the infection will spread if you mistake them for corns or calluses and touch them.
Athlete’s Feet (Tinea Pedis)



There are three types of athlete’s feet:
(1) Vesicular Scales (moist type): Reddish small vesicles develop in the sole and the toes, the epidermis dries in days, and the skin is peeled off. Even if the vesicles disappear, new ones develop in other areas.
(2) Interdigital Tinea (moist type): It often develops between the adjacent fourth and fifth toes. The skin is wrinkled in white, and is peeled off. The wrinkled area is expanded.
(3) Cornification (dry type): The whole sole, in particular, the heel, is cornified, the surface becomes rough, and the skin is peeled off.
In a severe case, it cracks. This type of athlete’s feet may not be often noticed, and it can be said that it can become easily chronic.
- Causes
- Trichophyton is a relative of mycete called filamentous bacterium, i.e., fungus, and eats skin protein (keratin) to live.
It is said that it multiplies at a temperature of 15 degrees Celsius and at 70% humidity or more. - Prevention and Measures
- It is important to always keep the feet clean (by washing and drying). They are indigenous bacteria, and there are a lot of chances of infection at public baths and sports club, where we walk barefoot, and at hospitals and hotels, where we share slippers, but it takes more than 24 hours to be infected after the attachment of bacteria. After you go to public baths or pools, use soap to wash your feet carefully. Infection can be prevented.
There are also many domestic infections, and you must be careful that you do not share a bath mat with germ carriers and that you do not walk barefoot in your house. Humid shoes become the hotbed of Trichophytons. Once you wear shoes, they become moist and it will take a whole day to dry them out. Try to wear at least two pairs of shoes by turns, and, when you wear shoes on one day, dry them in shade on the following day.
Moreover, once infected, it is necessary to continue applying medicine with patience. Make sure to apply the medicine to the whole foot since bacteria move around.
Some athlete’s feet may or may not accompany itchiness. Do not leave them just because they are not itchy, and make sure to undergo a dermatological examination. Even if symptoms look like those of athlete’s foot, there is a possibility of other skin diseases. If you feel something unusual with the skin, please be sure to consult a dermatologist.
Onychomycoses

Trichophytons come into the nails and multiply, and white turbidity, yellow turbidity, tylosis, and wavy or irregular deformation of the nails are observed.
Due to lack of subjective symptoms, many older people think that white turbidity and tylosis of the nails are symptoms of aging, and lack of awareness of the disease often lead to domestic infections.
The nails are important in that they support the toes while running.
If you leave tinea unguium, the feet may be easily exhausted and the shoes may become ill-fitting. Furthermore, the infection may spread to others.
- Causes
- (1) Leaving tinea pedis multiplies Trichophytons, and they further develop tinea unguium.
(2) Trichophytons come inside from sites of injury in the nails. - Prevention and Measures
- Antifungal agents are used for tinea, and there are two types of antifungal agents: external and internal medicine.
It is difficult to cure onychomycoses only with external medicine, and it is necessary to use internal medicine.
When you feel something unusual with the color and thickness of the nails, do not leave them and immediately consult a dermatologist.
Plantar keratoderma
The skin of the sole, in particular, of the heel, is dry, and it looks like it is powdery.
It may severely crack and may accompany pain or bleeding.
- Causes
-
(1) The dryness of the sole.
(2) Infections of Trichophytons. (Often they are not noticed.) - Prevention and Measures
- If the disease is caused by Trichophytons, use a cream containing anti-bacterial agents.
(Your dermatologist will give you the prescription)
In other cases, a cream containing urea is recommended.
It is recommended that you use slippers at home rather than living barefoot.
You must be careful that you should not share slippers with others.
Allergic Dermatitis
It refers to a condition where vesicles or red dots are found on the feet or the skin is wrinkled and peeled off, and it sometimes accompanies itchiness.
- Causes
- It is thought that it is caused by food, sweating disorders, stress, etc., and shoe-related causes are listed below:
1. The use of the rubber sole: Reaction to adhesives including rubber soles and rubber.
2. Allergy caused by chrome salt in tannic agents.
3. Dermatitis caused by dyes.
4. Allergy caused by materials used for the tiptoe and lining and by unbreathable shoes. - Prevention and Measures
- 1. For the rubber sole, shoes with the polyurethane sole are recommended.
2. Avoid leather products and use products made by canvas or artificial leather.
3. Avoid black shoes, as phenyldiamine used for dyeing is often used in black shoes. Also,
avoid brown shoes, as azo yellow materials are often used in brown shoes.
4. Preferably, try to select well-fitting shoes made by natural materials.
Ingrown Toenails

The side of the nail plate cuts into the nail fold to the side of nail groove, and inflammation develops around the area.
It develops reddening, swelling, and pain, and may form proud flesh.
- Causes
-
(1) Congenital factors.
(2) Ill-fitting shoes (including sports shoes).
(3) Habit of paring nails to the quick.
(4) Rolling caused by Trichophytons. - Prevention and Measures
- Make sure not to pare nails to the quick, and avoid walking and doing vigorous sports for a long time with ill-fitting shoes on. Please seek medical treatment if there is any nflammation.
Ingrown Nails

The nail and its surrounding soft tissue is pressured from outside, inside, and the tip of the nail, the nail plate is curbed transversely and rolled like a sheep horn, and ingrown nails sometimes accompanies strong pain.
They may inflame or may form proud flesh.
- Causes
-
(1) Congenital anomalies in the nail plate and the nail fold.
(2) Ill-fitting shoes (including sports shoes).
(3) Habit of paring nails to the quick.
(4) Rolling of the nail caused by tinea unguium. - Prevention and Measures
- Avoid walking and doing vigorous sports for a long time with ill-fitting shoes on.
Make sure not to pare nails to the quick, and always keep the feet clean.
When inflammation or complication of Trichophyton has been developed, please undergo appropriate medical treatment.
Pincer Nails
As in ingrown nails, while they are severely rolled, both sides of the nail may become stuck together to become tubular.
- Causes
- As in ingrown nails, causes are said to be mainly congenital.
- Prevention and Measures
- Pincer nails may be corrected if you properly cut the nails and remove the stiff nail fold.
A complication of tinea unguium has often been developed, and, in such a case, undergo medial treatment for tinea.
When they are severely rolled, you may mount a correction wire. However, this applies only to healthy and strong nails.
There is also a report saying that, if you stop correction, they may easily return.
Diabetic Foot Disorders
It is said that one sixth of patients with diabetes have disorders in the feet.
●Calluses and corns: Among patients with diabetes, they tend to frequently develop and acutely become big in comparison to healthy people.
●Dryness, crack, and recessus of the skin: Due to sweating disorders, the feet are unusually dry, and abnormal cornification and the crack of the skin develop.
●Ulcers: They often develop from blisters and wounds caused by wearing ill-fitting shoes. They scarcely accompany pain, and easily develop gangrene.
●Bone and joint diseases: They easily develop deformation of bones, which consequently develop calluses, ulcers, and so on.
- Causes
- (1) Peripheral circulatory disorders
The supply of nutrition to the part worsens. Once a wound is developed, a recovery disorder will be caused, and infectious diseases will easily develop from a small wound, which will further develop gangrene.
(2) Neurological Disorders
Since sensory, motor, and autonomic nerves are harmed, a small wound will easily become big without noticing the development. - Prevention and Measures
- Carefully choose well-fitting shoes, and be sure to wear socks to prevent frictions.
It is important to observe your feet every day and check whether there is any wound and so on.